Billing in cardiology is no longer just about sending claims; it’s about protecting your revenue in an era of tighter payer scrutiny. In 2026, bundled payment models and stricter payer rules are reshaping how cardiology services get reimbursed. For example, when a clinic visit happens on the same day as an echo, stress test, or cath, payers immediately ask: Was there a clear, separate medical need for both? If your documentation doesn’t make that distinction, payment is at risk of being bundled or denied.
This blog gives you a practical roadmap for navigating these challenges. We’ll cover the latest rules on bundling, how to choose the right E/M level, when to apply modifiers like 25 or the X{EPSU} family, and how to manage global periods. You’ll also see a simple workflow to run NCCI checks before claims go out, plus plain-language chart examples you can use in your notes right away.
E/M stands for Evaluation and Management. It is the visit you bill when you see a patient, ask questions, examine them, and make care decisions. In cardiology, E/Ms often happen on the same day as tests or procedures (like an echo, stress test, or cath). When you bill both a visit and a method, payers verify whether those services were separate and necessary. If they were not clearly separate, the claim can be denied or the payment bundled into the procedure. This makes correct documentation, including a clear review of system and the use of modifiers accurately and consistently, very important.
Here are examples you see every day:
These procedures often have their own payment rules and sometimes include a limited amount of physician work that could overlap with an E/M. Know the CPT-level cardiology billing codes for the procedure and whether the procedure’s payment already assumes part of the visit work. Many coding guides and vendor procedure guides list the most used cardiology codes for 2026.
Bundling means the insurer pays one combined amount instead of two separate payments. In the current healthcare landscape, bundled payments and bundled payment healthcare contracts (including Medicare bundled payments) make this even more important: payers increasingly expect a single, global payment for a package of services. If a procedure payment already covers time or work that is the same as the E/M, the insurer will bundle the E/M into the procedure.
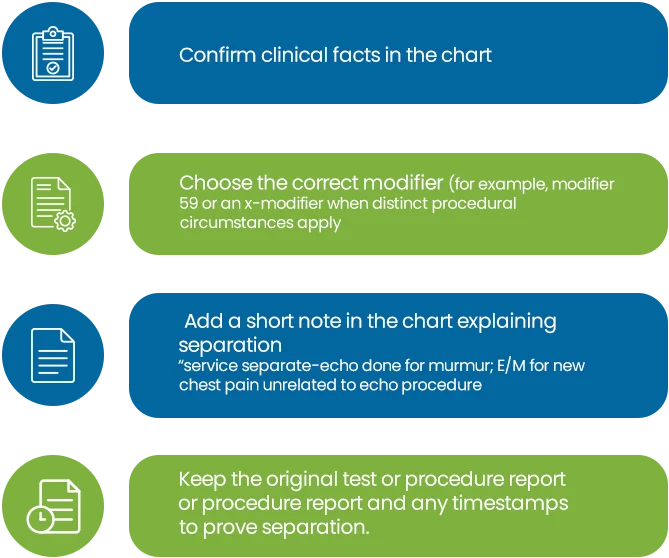
To bill the E/M service separately, you must demonstrate that the visit was a distinct service, not just a routine preoperative discussion or a routine explanation of the procedure. Use good notes and the right modifiers when appropriate. NCCI edits and payer bundling policies tell you which bundling services are not paid together under typical rules.
We help cardiology practices correctly apply E/M and procedure bundling rules to reduce denials and increase reimbursements.
When something is distinct and should be paid separately, modifiers can help. Use them only when the note truly supports separate services.
Pick an E/M code in two ways: by MDM (medical decision making) or by time. Use the rule that applies to your visit.
NCCI (National Correct Coding Initiative) rules tell Medicare which code pairs are not paid together. These edits stop payments for services that overlap. Run an NCCI check in your billing system before you send claims.
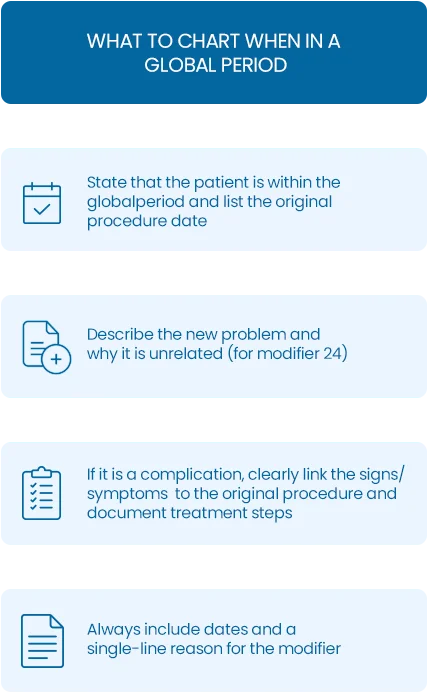
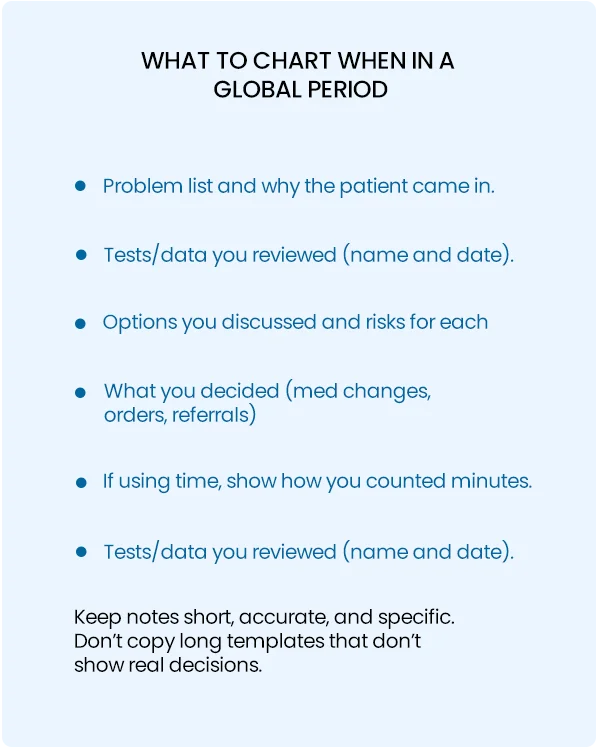
Some cardiology procedures (like device implants) have a global period. That means routine care after the procedure is included in the payment for the procedure.
When it’s okay: If the clinic visit had a separate, significant medical reason (new chest pain, medication change, acute shortness of breath) that required independent decision making, you may bill both the E/M and the echo. Use modifier 25 on the E/M and document the separate reason. Put one brief sentence that shows the separation, and list the tests you reviewed. Example chart line:
“25 appended, E/M for new-onset exertional chest pain; echo performed for murmur. E/M addressed medication change and risk discussion; echo for structural assessment.”
When it’s not okay: If the visit was only routine prep for the echo (talking about the test, consent, basic instruction), do not bill a separate E/M. That work is part of the procedure and may be considered part of bundling services under payer rules.
Many cath codes include pre-procedure evaluation. That means the payment for the cath often already covers some pre-op physician work. Do not routinely bill a separate pre-op E/M unless the visit involved a real, separate evaluation with distinct decisions (for example, solving an acute new problem or making a major change in care). If you do bill separately, document why the visit was distinct and check NCCI edits for the specific code pair. Example chart line:
“Pre-procedure consult was for evaluation of new syncope and anticoagulation plan change before cath, E/M distinct from cath work; see problem list and medication changes.”
Cardiology billing in 2026 is more than just knowing the codes; it’s about clearly and completely telling the story of your patient encounter. When an E/M visit and a procedure occur on the same day, payers will always look for overlap, particularly as Medicare’s bundled payment programs expand. If your documentation proves the services were distinct, you protect both your compliance and your revenue.
The keys are simple: select the right E/M level, understand which procedures often bundle, use modifiers carefully (only when justified), and always run NCCI checks before submitting claims. Document the “why” behind your decisions, whether it’s a new complaint, a change in care, or a complication, and make sure your review of systems is clear and targeted. Use accurate cardiology billing codes, and consider partnering with trusted cardiology billing services if you need assistance.
By applying these steps, your practice can reduce denials, shorten payment delays, and safeguard revenue streams. Most importantly, it frees you to spend less time on billing headaches and more time focusing on what matters most: delivering excellent care to your patients.
Leverage AI for faster claims, reduced denials, and improved reimbursement.
Please provide the following information, so our team can connect with you within 12 hours.
Or call us as 800-640-6409