In the U.S., the medical insurance claim process is notoriously complex and prone to errors that cost healthcare providers billions each year. Consider that nearly 15% of all claims submitted to private payers are initially denied. Hospitals spent roughly $19.7 billion in 2022 just to appeal and correct denied claims, which is an immense financial drag. Moreover, industry data shows that as many as 60% of returned claims are never resubmitted, meaning lost revenue that practices never recover. This is where clean claim submission plays the most important part.
By submitting “clean” claims (i.e., error-free and complete) from the very start, providers can improve their overall revenue cycle, and avoid the costly penalties, denials, and rejection appeal process. In fact, clean claim submission on the first time is frequently identified as the optimal way to increase payment percentages and minimize the duration of the revenue cycle.
What is Clean Claim Submission?
A clean claim is a health insurance claim that is complete and correct the first time it’s submitted. In other words, the claim has no errors, missing information, or problems that would delay payment. One official definition says a clean claim is a submitted claim without any errors or issues (including missing documentation) that delay timely payment. This means all the needed data is there and accurate.
For example, a clean claim correctly includes the patient’s information, the provider’s details, the dates of service, the procedure codes, the diagnosis codes, and any required documents. The insurance company can process it without coming back to the provider for corrections. If a claim has a mistake (like a wrong code or missing patient birthdate), it’s not “clean” – it might be rejected or denied until it’s fixed.
Clean claim submission is the goal of sending out only clean claims. It’s like handing in a perfect homework assignment that the teacher (insurer) accepts right away. Clean claims “fuel your practice’s revenue and cash flow” because they get approved faster. Next, we’ll see why clean claims are so important for a healthcare practice’s financial success.
To break down the concept of clean claim submission if only it checks all the following criteria.
- Correct Provider and Facility Information: Identifies the provider (and facility, if applicable) with all required identifiers (e.g., NPI).
- Accurate Patient and Insurance Details: Patient demographics and insurance policy details are complete and verified (confirming coverage eligibility).
- Proper Dates and Service Codes: Includes the correct date/place of service and properly coded procedures (CPT, HCPCS, ICD-10), all of which must be covered under the patient’s plan.
- Medical Necessity & Documentation: Services are medically necessary and backed by proper documentation (attach notes, test results, prior authorization references as required).
- Compliance with Payer Rules: Follows any payer-specific rules (correct modifiers, form, etc.) and is submitted within the timely filing window (e.g., within 90 days to 6 months of service, depending on the insurer).
- No Technical Errors: All required fields are filled with the correct formatting, accurate IDs/codes, and no duplicate claims for the same service.
Submitting a claim that meets all these criteria is essentially the goal of clean claims medical billing best practices; in other words, it’s about “getting it right the first time.” This clean claim submission approach streamlines the process by preventing avoidable hiccups like rejections or requests for more information, extra documentation or any other paperwork.
By paying attention to each of the claim processing steps in an efficient medical billing process; from patient intake and insurance verification to coding and final review, a healthcare practice can achieve a high rate of clean claims submission. Now that we understand what it means to submit clean claims, let’s explore ten key reasons why clean claim submission in medical billing is so vital for the financial and operational health of your medical practice.
10 Reasons Why Clean Claim Submission Is Important for Your Practice
Faster Reimbursements and Improved Cash Flow
Using clean claims medical billing helps insurers pay you faster, which boosts your practice’s cash flow. When a claim has the right CPT and ICD-10 codes, the correct NPI, and passes the clearinghouse EDI 837 scrub, it glides straight to the payer’s computer. Their auto-adjudication system can okay it without extra back-and-forth or 277 correction messages. Many states have prompt-pay rules that say insurers must send an ERA and EFT within 30–45 days once a claim is clean, so getting it right the first time means cash arrives on time. This steady revenue pays daily costs and lets you buy new lab gear. Quick, accurate claims keep your practice stable and ready to grow.
Comparative Impact of Claim Quality on Revenue Velocity
| Revenue-Cycle Scenario | Average Days-to-Payment | Denial / Rework Rate | Net Collection Rate | Month-End Cash Position |
| Streamlined “Express Lane” (Clean Claim Submission) | 14 day | 2% | 98 % of total charges | USD 200,000 |
| Delayed “Congested Lane” (Error-Prone Submissions) | 45 days | 12% | 85 % of total charges | USD 140,000 |
Illustrative figures for a mid-sized multispecialty practice that bills USD 250,000 in services per month. The comparison demonstrates that clean claim submission is analogous to keeping revenue in an “express lane,” ensuring predictable, expedient, and maximized cash flow for the practice.
Higher First-Pass Approval Rates (Fewer Denials)
One big reason to use clean claims medical billing is that it cuts claim denials way down. Experts say 85–90 % of denials could be stopped if the front-end work—like checking codes and patient data were done right. Sending clean claims is the smartest way to avoid those denials. When you fix easy errors, such as missing ICD-10 codes or wrong modifiers, most claims earn a high first-pass approval rate, so they pay the first time and need no fixes. That puts more money straight on your bottom line, because a claim paid on first pass never risks going unpaid. (Remember, about 65 % of denied claims are never sent in again, so that money is lost for good.)
Case Study
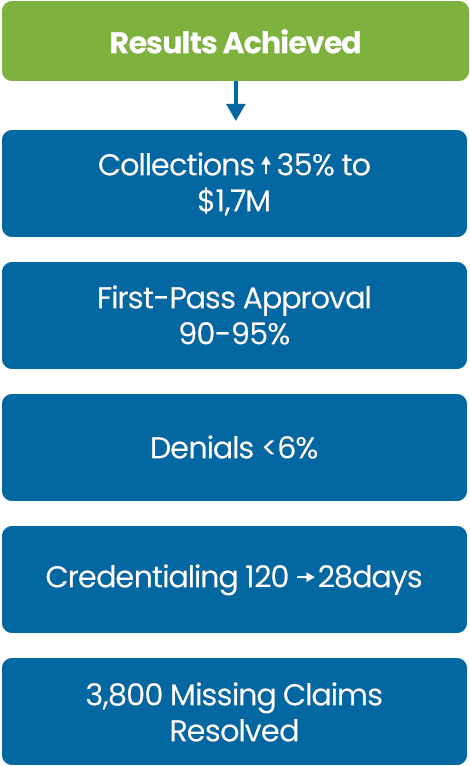
Spine & Wellness Center of America, a nine-physician pain-management group in South Florida handling more than 140,000 encounters annually, had plateaued at USD 1.3 million in monthly collections, with only 60–65 percent of claims paid on first pass. Denials stemmed from overdue Medicaid revalidations, clearing-house ID mismatches, inconsistent CPT/ICD coding, and thousands of unreconciled superbills.
After outsourcing revenue-cycle operations to MedCare MSO, the practice underwent a six-month overhaul deadline-driven credentialing, repaired EDI links, unified clearing-house feeds, dual coding audits with clinician training, daily charge-capture reconciliation, and streamlined claim submission in medical billing workflows.
Lower Administrative Costs and Workload
When you use clean claims medical billing, you make more money and spend less on paperwork. A single denied claim can cost about $25 in staff time—that’s people looking up the mistake, fixing the ICD-10 or CPT code, and sending the claim through the EDI clearinghouse again. Those dollars add up fast. Clean claims stop that waste. Because there are fewer coding errors and fewer appeals, your billing team can focus on work that actually earns money, like following up on current patient accounts or giving patients a better billing experience. In short, sending clean claims makes your whole medical-billing process much cheaper and far more efficient than constantly fixing avoidable errors.
Reduce Denials And Delays
Accurate submissions speed payments and minimize unnecessary follow-ups.
Shorter Accounts Receivable Cycles
Using clean claims medical billing from the start makes money come in quicker. If each claim lists the right CPT and ICD-10 codes, the correct NPI, and passes the EDI 837 check with no mistakes, it moves straight to the payer’s computer. Because nothing needs fixing, the payer sends the ERA and EFT in just a couple of weeks instead of many months. That lowers your Days in A/R and puts cash in the bank faster, so you do not hit cash-flow crunches. Quick payments help you cover payroll, buy lab supplies, and even add new tests without borrowing. In short, clean claims speed up the whole medical-billing insurance claims process and make your practice’s income steady, healthy, and ready to grow.
Compliance with Regulations and Payer Policies
With clean claims medical billing, sending in accurate claims keeps your practice safe with the rules. Health billing must follow many laws like HIPAA privacy, Medicare/Medicaid billing rules, and state insurance laws and every private payer has its own guidebook. If a claim has the wrong code or missing info, it can set off compliance alarms. Submitting correct claims with the right CPT and ICD-10 codes, solid notes to show medical necessity, and any needed authorizations proves you are honest and helps prevent fraud or abuse troubles.
Moreover, when you use clean claims medical billing, payers must follow prompt-payment rules and must pay a clean claim within a set number of days. Sending clean claims all the time also lowers your chances of outside audits and big fines. In short, clean claims keep your practice on the right side of the law and make the whole claim-submission process easy to understand and track.
Avoidance of Timely Filing Denials and Lost Revenue
Missing a payer’s deadline is one of the most expensive billing mistakes a practice can make. Most insurers give you 90 or 180 days from the date of service to get a claim received—not just sent. If the claim goes out with errors, it can be kicked back while the filing clock keeps ticking. By the time you fix and resubmit, you might pass the deadline and see the denial code “Exceeded timely filing limit.” When that happens, the payer owes you nothing.
Using clean claims medical billing is the best way to beat this problem. A claim that’s correct on the first pass almost never bumps into timely-filing limits. That’s vital for small practices that can’t afford to write off whole visits just because the paperwork was late. In short, clean claims act like an insurance policy against losing revenue to avoidable filing delays, protecting every dollar your practice earns.
Improved Operational Efficiency and Staff Productivity
Focusing on clean claims medical billing puts a hierarchical order in your revenue-cycle work. Because claims go out right the first time, your billing team deals with fewer fixes and can follow a steady, easy-to-repeat routine. This boosts their daily productivity and lets the system grow with your practice without swamping the staff. Deploying automated claim-scrubbers and holding routine coder-training sessions safeguard accuracy across the board—from patient demographics to CPT and ICD-10 entries. Nail the details up front, and your team works smarter, not harder, while sidestepping headaches later on.
Better Provider-Payer Relationships
Submitting clean claims medical billing can even make life easier with insurance payers. When your practice always sends complete, accurate claims, payers like it because they spend less time fixing mistakes. Over time, they see your office as “easy to work with,” so calls with insurer reps feel friendlier and problems get solved faster.
This good payer name benefits you when you require something extraordinary like renegotiation of a rate on a contract or appeal of a tough case because payers trust your paperwork. Even some insurers offer incentives in terms of quicker settlement of claims or minuscule bonuses to providers who have low error rates. In short, clean claims build confidence with payers and keep the business side of healthcare running smoothly.
Enhanced Patient Satisfaction and Transparency
Even though patients don’t see and know the medical billing procedure, they definitely feel its effect with a smooth payment clearance process. When your practice uses clean claims medical billing—meaning claims go to the insurer right, the first time, patients get clear, accurate bills (and explanations of benefits) fast. That cuts down on confusion and stress because they aren’t billed for services insurance should cover, and they aren’t hit with surprise statements months later while an insurance fight drags on.
A smooth billing flow also boosts how patients view your office. Long delays or repeated billing mistakes can chip away at trust, but quick, error-free invoices build confidence and goodwill. Bottom line: clean claims lead to straightforward, timely communication about costs and that raises patient satisfaction with your entire practice.
Stronger Financial Performance and Practice Growth
Using clean claims medical billing keeps money coming in so your practice can grow. When claims go out error-free, insurers pay faster, collections rise, and staff spend less time fixing mistakes so costs drop. With extra cash on hand, you can hire more team members, buy new lab machines, or add services. Clean claims also give you better data for planning because the numbers are accurate. In a field with tight budgets, getting claims right the first time is a key step to long-term success and steady financial health even when times get tough.
Increase Claim Acceptance Rates
We handle your clean claim submissions, ensuring compliance, accurate coding, and faster reimbursement for your practice.
Actionable Tips for Ensuring Clean Claims
Achieving a high clean-claim rate takes a concerted effort. Here are a few actionable tips to improve your claim processing steps in healthcare billing workflows:
| What to Do | How It Works (in simple words) |
| Train your team often | Make sure coders and billers learn the newest ICD-10 and CPT rules plus each payer’s special edits. Quick refresher classes stop mistakes before they start. |
| Let smart software help | Use your EHR or a claims program with a built-in claim scrubber. It scans each form for missing info or bad codes and flashes a warning so you can fix it fast. |
| Check insurance first | Before the test or visit, run an eligibility check and grab any needed prior authorizations. Catching coverage problems early keeps claims from being denied later. |
| Do a mini audit before you hit “send” | Use a short checklist: right patient name, correct modifier (like -26 for the pro part), matching dates, and no blank boxes. One extra look on Day 1 can save weeks of delay. |
| Watch your denials like a hawk | Track every denial reason. If “wrong code” pops up again and again, dig in, find the cause, and fix the workflow. Learning from mistakes pushes your clean-claim rate higher over time. |
Follow these steps and your practice will file cleaner claims, get paid faster, and spend less time untangling billing errors.
Conclusion:
Clean claim submission might sound technical, but it boils down to a simple idea: get it right the first time. For healthcare providers focused on financial performance and compliance, mastering clean claims is incredibly important. When you send out accurate, complete claims, you speed up reimbursements, reduce denials, and maintain a healthy cash flow for your practice. It also keeps you in good standing with insurance regulations and requirements.
In summary, a clean claim is one with all the t’s crossed and i’s dotted – correct patient info, correct codes, necessary documents, and no mistakes. Achieving a high clean claim rate requires attention to detail, good training, and the help of technology (like clearinghouses and scrubbing tools). The effort is well worth it. With clean claims, you spend less time fixing billing errors and more time focusing on patient care and practice growth. It’s like having a well-oiled machine in your billing department – everything runs smoother.
By applying the strategies outlined above and fostering a culture of accuracy and compliance, healthcare practices can significantly boost their revenue cycle success. Clean claims mean the money you earn finds its way into your pocket faster and with less resistance. For any provider or clinic aiming for financial stability and efficiency, paying close attention to clean claim submission is a smart and necessary move. After all, you’ve provided the care – a clean claim ensures you get paid for it swiftly and fully.