The future of medical coding and billing trends shows that the healthcare industry is growing. As it grows, so does the number of complex regulations and requirements governing practitioners.
Let’s face it. It is hard to think about the future of your business and profession when most of you are just trying to get through the day’s workload while still providing quality care.
It’s tough, right?
However, the good news is that medical billing is expected to change in the future due to the use of emerging technologies, such as artificial intelligence (AI), automation, and blockchain technology.
In this blog, we are going to explore the history of medical billing, its evolution, and future predictions. By the end of this article, you will have a clear picture of the future of medical billing and what you exactly need to adopt to grow your practice.
So, without any further ado, let’s dive into the world of medical billing!
How Did We Get Here?
Imagine trying to keep track of your doctor visits, tests, and bills on paper. That’s how medical billing used to be! It was slow, easy to lose, and had lots of mistakes.
Then came computers. Electronic Health Records (EHRs) replaced paper files. This made it easier to find information and share it with insurance companies. But there was still a lot of manual work to do.
Keeping track of medical records manually was undoubtedly challenging. It required significant time for medical staff to review health records, separate treatments, and procedures, assign costs, and prepare the final bill.
Today, advanced software and hardware enable rapid billing processes, with results available almost instantly. Consequently, healthcare facilities that do not adopt medical billing software risk falling behind.
From Paper to Digital: The Advent of Electronic Health Records
The Regenstrief Institute introduced the first electronic medical records (EMR) in 1972, marking a major leap forward for the healthcare sector. However, due to the high costs, this innovation did not gain widespread adoption initially.
It wasn’t until the American Recovery and Reinvestment Act of 2009, which included incentives for adopting EMRs, that medical facilities began transitioning to digital records.
Are EMR and EHR the Same?
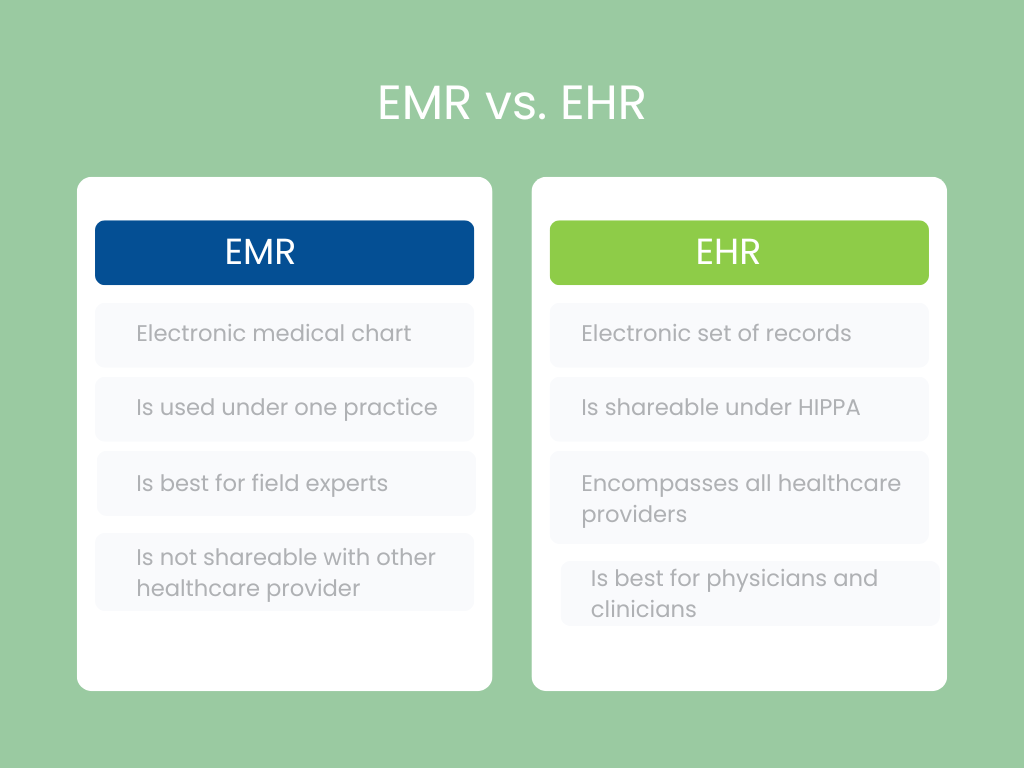
While the terms EMR (Electronic Medical Record) and EHR (Electronic Health Record) are often used interchangeably and refer to similar systems, there is a distinction. EHR is a broader term that includes a wider range of health information, whereas EMR is more specific to individual practices. For most healthcare providers, both terms represent the shift from paper-based records to digital systems.
The widespread adoption of EHR and EMR systems is crucial for advancing healthcare in general.
Where Are We Now?
Changes can also be seen in how we bill for medical care and even how those services are reimbursed. Services that previously required significant overhead and in-practice support are being streamlined, and remote or third-party medical coding and billing services are growing. And that growth is expected to continue as medical front offices find a new equilibrium, embracing trending services and simple tools to help small medical practices redefine their customers’ needs.
The Bureau of Labor Statistics forecasts that the need for trained medical billing and coding experts will grow by 9% over the next decade. This is partly due to a growing United States population and the fact that Americans are living longer. With a strong need for medical bills, technological developments take center stage.
Within the past two decades, electronic claims processing and medical billing have transformed the healthcare industry. With few exceptions, state and federal laws now require providers to utilize electronic records management and claim transmission systems.
Today, we have special software that helps with medical billing. It’s like a smart helper that does a lot of the boring work.
What Are the Benefits of Electronic Health Records?
EHRs are crucial for managing and accessing patient medical histories effectively. Their benefits include:
- Facilitating communication between healthcare providers across different settings and providing quick access to patient records.
- Automatically detecting and alerting healthcare professionals about medication allergies and potential drug interactions.
- Enabling doctors to swiftly review a patient’s extensive medical history.
- Minimizing errors caused by poor communication or illegible handwriting.
For instance, when a physician needs to assess the best treatment for a patient’s new symptoms, EHRs enable them to easily review years of medical history. The system may also suggest treatment options or indicate if a proposed treatment is unsuitable. Additionally, EHRs can alert the doctor to potential drug interactions or allergies and check whether the treatment is covered by insurance. The doctor can then send the prescription or order electronically.
When used effectively, EHRs enhance patient care by making management more efficient and accurate.
Curious how modern billing solutions can help practice adapt faster?
What Are the Different Types of Electronic Health Records?
EHRs are used across various healthcare environments, including:
- Primary care providers such as doctors, nurse practitioners, and physician assistants.
- Medical groups with multiple locations and specialties.
- Hospitals and urgent care facilities.
- Health and dental insurance companies.
- Pharmacies.
- Laboratories.
What’s Next for Medical Billing?
Medical billing is about to change significantly due to new technology and evolving industry needs. Here’s what to expect:
1. Increased Automation
Automation will revolutionize medical billing by making it more efficient and cutting down on mistakes.
- Error Detection and Correction: Automated systems will increasingly handle routine tasks, such as spotting and fixing errors in billing codes. This means fewer mistakes and more accurate billing.
- Claims Processing: It will speed up the claims submission process, leading to quicker reimbursements for healthcare providers and fewer patient delays.
- Reminders and Notifications: Automated reminders will help both patients and providers stay on top of important billing dates, like payment deadlines and upcoming appointments.
2. Artificial Intelligence (AI)
Artificial intelligence (AI) is beginning to change not only how medical offices provide care but, more importantly, how billing codes are managed and reimbursed. An increasing number of insurance payers are using artificial intelligence to analyze large medical claims data sets for coding errors, anomalies, reimbursement fraud, and abuse.
Here’s how AI will play a big role in improving medical billing:
- Predictive Analytics: AI will analyze past billing data to estimate potential issues before they occur. This includes spotting patterns that might lead to claim denials or disputes.
- Cost Savings: AI will optimize billing practices by suggesting more efficient coding and practices, helping providers save money.
- Fraud Detection: Advanced AI will detect fraud by identifying unusual patterns and anomalies in billing data, helping to prevent fraudulent activities.
3. Enhanced Patient Portals
Patient portals will become more advanced and user-friendly. Here’s how:
- Billing Transparency: Patients will have clearer access to detailed billing information. It will help them understand charges, track payments, and review their statements.
- Online Payments: Integrated payment systems will make it easy and secure for patients to pay bills online, reducing reliance on paper statements.
- Communication: Patients will be able to resolve billing issues and ask questions through secure messaging features, improving communication with healthcare providers.
4. Blockchain Technology
Blockchain can provide enhanced transparency, traceability, and security, helping patients determine if they are consuming fake medicines. It will offer a new level of security and accuracy in medical billing. Here are some predictions we can expect for the future:
- Data Security: Blockchain’s encrypted, decentralized structure will protect sensitive medical and billing information from unauthorized access and tampering.
- Transparency and Accuracy: It will provide a transparent record of transactions, reducing disputes and billing errors.
- Interoperability: It will also enable better data sharing between systems and organizations, providing a unified and accurate record of patient information.
5. Impact on Stakeholders
Three important stakeholders in the medical billing sector include:
- For Patients: These changes will make billing more transparent, efficient, and secure. Patients will benefit from easier access to billing information, faster resolution of issues, and improved privacy.
- For Healthcare Providers: Automation and AI will simplify billing processes. It will cut down on administrative work and enhance financial performance by reducing errors and optimizing claims. Blockchain will boost data security and interoperability.
- For the Industry: Overall, these technological advancements will create a more efficient, accurate, and secure medical billing system. This will improve financial outcomes for providers, enhance patient satisfaction, and make healthcare administration more effective.
The Bottom Line
Healthcare is not going back to the days when billing, or any other process, was done manually. Instead, it is destined for a future in which AI and machine learning will become commonplace.
So, we can say that the future of medical billing is bright. These new technologies promise to make the system more efficient, accurate, and secure. The good thing? It benefits everyone involved.

