Credentialing is the process of verifying and validating a healthcare provider’s qualifications, licensure, training, and professional background before they are allowed to practice or bill insurers. For mental health professionals in the U.S. such as therapists, counselors, psychologists, and psychiatrists, proper credentialing is essential to join insurance networks (getting “paneled”), comply with regulations, and receive reimbursement for services. In other words, credentialing is the gateway to both trust and payment in mental healthcare. Without being credentialed with insurance companies or government payers (Medicare/Medicaid), providers generally cannot bill those payers for client sessions. This means delays or gaps in credentialing can lead to denied claims and substantial lost revenue for a practice.
Choosing a credentialing service, a third-party that handles this complex process on your behalf, can save mental health practices significant time and help avoid costly mistakes. To ensure smooth credentialing, selecting the best credentialing services for mental health providers is crucial for avoiding errors and delays. However, selecting the best credentialing service for mental health requires careful consideration of many factors, from the service’s expertise and cost to how it integrates with your billing processes.
This comprehensive guide breaks down everything you need to know to make an informed decision. We’ll cover how credentialing works, why it’s closely tied to billing, the pros and cons of in-house vs. third-party credentialing, and detailed criteria for evaluating credentialing service providers.
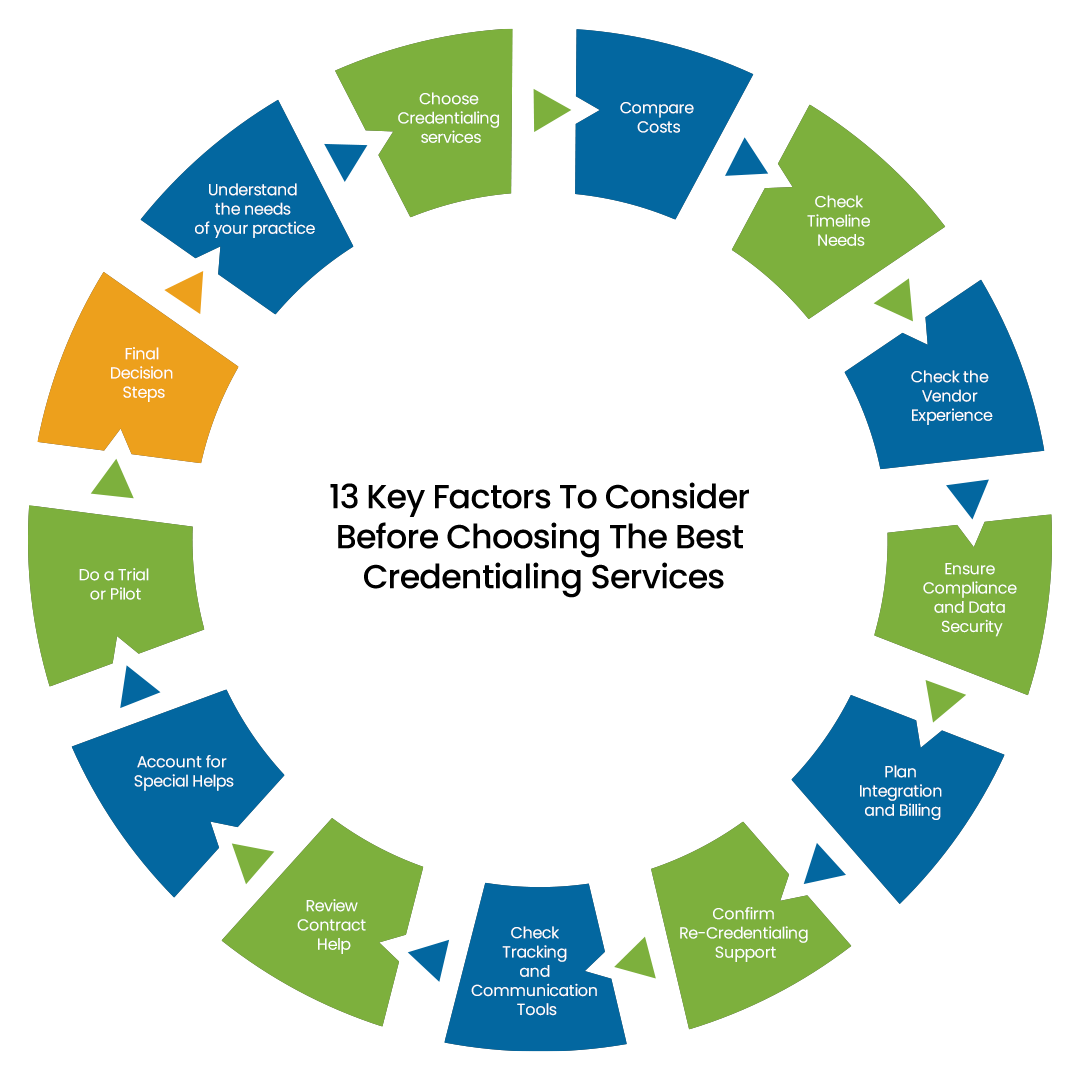
13 Key Factors To Consider Before Choosing The Best Credentialing Services
1-Understand the needs of your practice
2-Choose Credentialing services
3-Compare Costs
4-Check Timeline Needs
5-Check the Vendor Experience
6-Ensure Compliance and Data Security
7-Plan Integration and Billing
8-Confirm Re-Credentialing Support
9-Check Tracking and Communication Tools
10-Review Contract Help
11-Account for Special Helps
12-Do a Trial or Pilot
13-Final Decision Steps
Understand the Needs of Your Practice
Determine the number of providers who require credentialing first. Note down names and positions, such as counselors or therapists. Next, make a list of the insurers you would like to use, including private insurance, Medicaid, and Medicare. Planning mental health billing and credentialing is made easier with this list. Lastly, consider whether you need outside assistance or if your employees can do the task internally. The decision between in-house and third-party credentialing is crucial for getting off to a good start.
Choose Credentialing Services
If you pick in-house credentialing, your team handles all steps. Your staff gathers documents, fills out forms, and tracks status. In-house can save money for a small group, but it needs time and training. If you choose third-party credentialing, a vendor does the paperwork for a fee. Experts know mental health billing and credentialing rules and can avoid mistakes. Third-party help frees your staff for patient care but costs more. Think about how many providers you have, staff skills, and your budget when you decide.
Compare Costs
Compare the cost of in-house work to vendor fees. For in-house cost, calculate staff hours times wage, and add training time. For example, if someone spends 10 hours at $20/hour, that is $200 plus any training. For vendor cost, ask for flat fees or monthly fees and check if there are extra charges for renewals or new payers. For instance, a vendor may charge $300 per provider or $50 per month per provider. Put both numbers side by side. A small practice might find in-house cheaper. A larger practice may save time and reduce errors by paying for third-party credentialing. This step links directly to good mental health billing and credentialing budgets.
Cost Comparison: In-House Vs Third-Party Credentialing
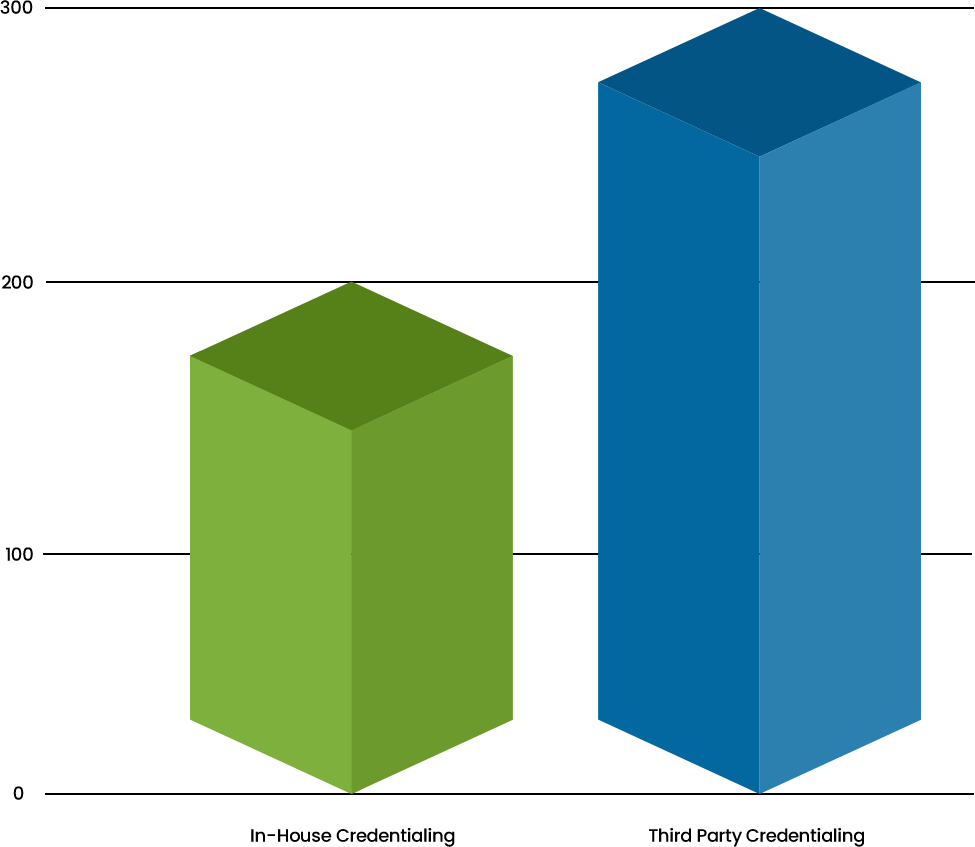
In-House Credentialing: $200 (10 hours × $20/hour)
Third-Party Credentialing: $300 (flat fee per provider)
Check Timeline Needs
Credentialing takes time. Each insurer often needs 60–120 days or more to approve a provider. Think about how soon you need new providers ready to bill. If you need faster results, a vendor’s experience may speed things up. If you have enough time before seeing many new patients, in-house can work. Plan ahead so you do not lose money waiting for approvals. Good mental health provider credentialing means starting early and avoiding gaps in billing.
Check the Vendor Experience
Examine their background with mental health professionals if you are thinking about getting third-party assistance. Find out whether they have previously assisted psychologists, counselors, or therapists. This guarantees that they are aware of the requirements for certifying mental health providers. Request references or reviews from similar practices. Ensure that the vendor supports CAQH profile management, a crucial tool for simplifying the credentialing process across multiple insurers. Contact those references to hear about real experiences. Also confirm the vendor knows rules for Medicare, Medicaid, and other insurers you listed. A vendor with proven experience will help your mental health billing and credentialing to move forward smoothly.
To check the experience and expertise in credentialing for mental health providers, you can ask following questions:
-How many years have you been credentialing for mental health providers?
-Which insurance companies or networks have you worked for credentialing mental health providers?
-What is your process for verifying the credentials of mental health providers?
-What tools or software do you use to manage the credentialing process?
-How do you ensure the accuracy and completeness of credentialing applications?
Ensure Compliance and Data Security
Your data must stay safe. Inquire about third-party vendors’ information security and adherence to HIPAA regulations. They ought to make advantage of encrypted storage or protected portals. Establish password-protected digital folders or lockable cabinets for internal work. Ensure that transcripts, license copies, and other documents remain confidential. Only share information with a vendor that shows clear security steps. This protects patients and keeps your mental health provider credentialing honest and safe.
Plan Integration With Billing
Credentialing and billing must connect. Decide how to tell billing staff when a provider is approved. It could be a dashboard check, system update, or email. Check to evaluate whether the vendor’s billing assistance saves time and effort. If you do in-house work, create a checklist such as “when credentialing finishes”, “input provider details into billing software”. This helps avoid claim rejections. Planning integration ensures your mental health billing and credentialing process flows without breaks.
Confirm Re-Credentialing Support
Credentialing does not end once. Providers must renew credentials every 1–2 years. Ask vendors if they remind you and handle renewals as part of the service. For in-house, set calendar alerts for license renewals and CAQH updates. Missing a renewal means you cannot bill. Good re-credentialing support keeps your practice running without gaps. This is a key part of mental health provider credentialing maintenance.
Check Tracking and Communication Tools
Tracking applications helps you stay on top of the process. A good vendor may offer an online portal or dashboard. There you can see status for each provider and payer. If you work in-house, use a simple spreadsheet. Include columns for provider name, insurer, date sent, status, and next follow-up date. Update this sheet weekly. Also decide who on your team checks status and who informs billing staff. Clear tracking and communication link credentialing actions to billing tasks.
Review Contract Help
Payer contracts include rates and terms. Some vendors review these contracts to ensure they are fair. This can help you know if a contract covers your costs. If you do in-house work, find someone who can read and explain contracts or get outside advice. Knowing contract start dates ensures you bill at the right time. Good contract review support fits into mental health billing and credentialing by avoiding surprises.
Account for Special Needs
If your practice offers telehealth, credentialing rules may differ. Check if the vendor or your team knows extra steps for virtual care. Some insurers have special forms for telehealth. If you add new services like group therapy or new license types, verify credentialing requirements. A vendor with mental health billing and credentialing expertise can guide you through these changes. Planning for special needs keeps your credentialing current as your practice grows.
You can ask them these questions to be clear about their scalability:
-How do you manage an increase in the number of your clients?
-Can your credentialing services be scaled up or down based on our needs?
-How do you plan to see future growth and changes in the healthcare industry?
Do a Trial or Pilot
Before full commitment, test one approach. For in-house, credential one provider with one or two insurers. Note how long it takes and if errors occur. For a vendor, ask them to credential one provider first. Observe their speed, communication, and security. Compare results. This trial helps you decide whether in-house or third-party credentialing fits best. Learning from a small test avoids big problems later.
Final Decision Steps
Gather all information: cost estimates, timeline needs, tracking tools, and vendor details. Talk with your team about time and skills. Check vendor data security, experience, and support for mental health billing and credentialing. List pros and cons for in-house vs third-party credentialing. Choose the option that fits your budget, staff capacity, and practice size. Then make a clear plan: who does each task, deadlines, and how billing is notified. Document the plan so everyone knows their role. This final step ensures smooth mental health provider credentialing.
Conclusion
Choosing the best credentialing service is about knowing your needs, costs, time, and skills. Follow these steps to link credentialing with mental health billing and credentialing. Decide between in-house vs third-party credentialing by comparing benefits and costs. Keep data secure, plan integration with billing, and arrange for renewals. Use tracking tools and test options if unsure. With a clear plan in place, you can focus on patient care while credentialing runs smoothly behind the scenes.

